Glioblastoma (GBM) is a highly invasive cancer of the brain and spinal cord. Brain cancers like GBM are challenging to treat because many cancer drugs cannot pass through the blood-brain barrier. In addition, although surgery and subsequent chemotherapy and radiotherapy are the most successful methods to treat the disease, more than 90% of GBM tumors will relapse after surgical resection.
In a new study led by researchers at Brigham and women's Hospital and Harvard Medical School, scientists designed a new treatment strategy to treat postoperative GBM by using stem cells from healthy donors to attack GBM specific tumor cells. This strategy showed great efficacy in the preclinical model of GBM, with 100% of mice living beyond 90 days after treatment. The findings will be published in nature today.
"This is the first study to our knowledge, which identifies the target receptors on tumor cells before starting treatment, and uses biodegradable, gel encapsulated, 'off the shelf' engineered stem cell-based treatment after GBM tumor surgery," said Khalid Shah, director of the stem cell and translational immunotherapy Center (CSTI), deputy director of research in the Department of neurosurgery in Brigham, and a teacher of Harvard Medical School and Harvard Stem Cell Institute (hSCI), "In the future, we will apply this strategy to identify the target receptor in time after people receive the GBM diagnostic results, and then apply the gel encapsulated, off the shelf engineered stem cell therapy from the pre manufactured reservoir."
Many cell-based cancer treatments come from patients' own stem cells or immune cells. However, in diseases such as GBM, due to the rapid development of the disease, most patients undergo surgery in the first week after diagnosis, and there is little time to develop treatments from their own cell types. Instead, scientists have developed a novel method that uses allogeneic stem cells or cells from healthy people to provide immediate remedies during surgery. Shah and colleagues evaluated the efficacy of several capsules that carry stem cell therapy in the brain, and also found that a biodegradable hydrogel capsule can successfully deliver the treatment without being washed away by cerebrospinal fluid.
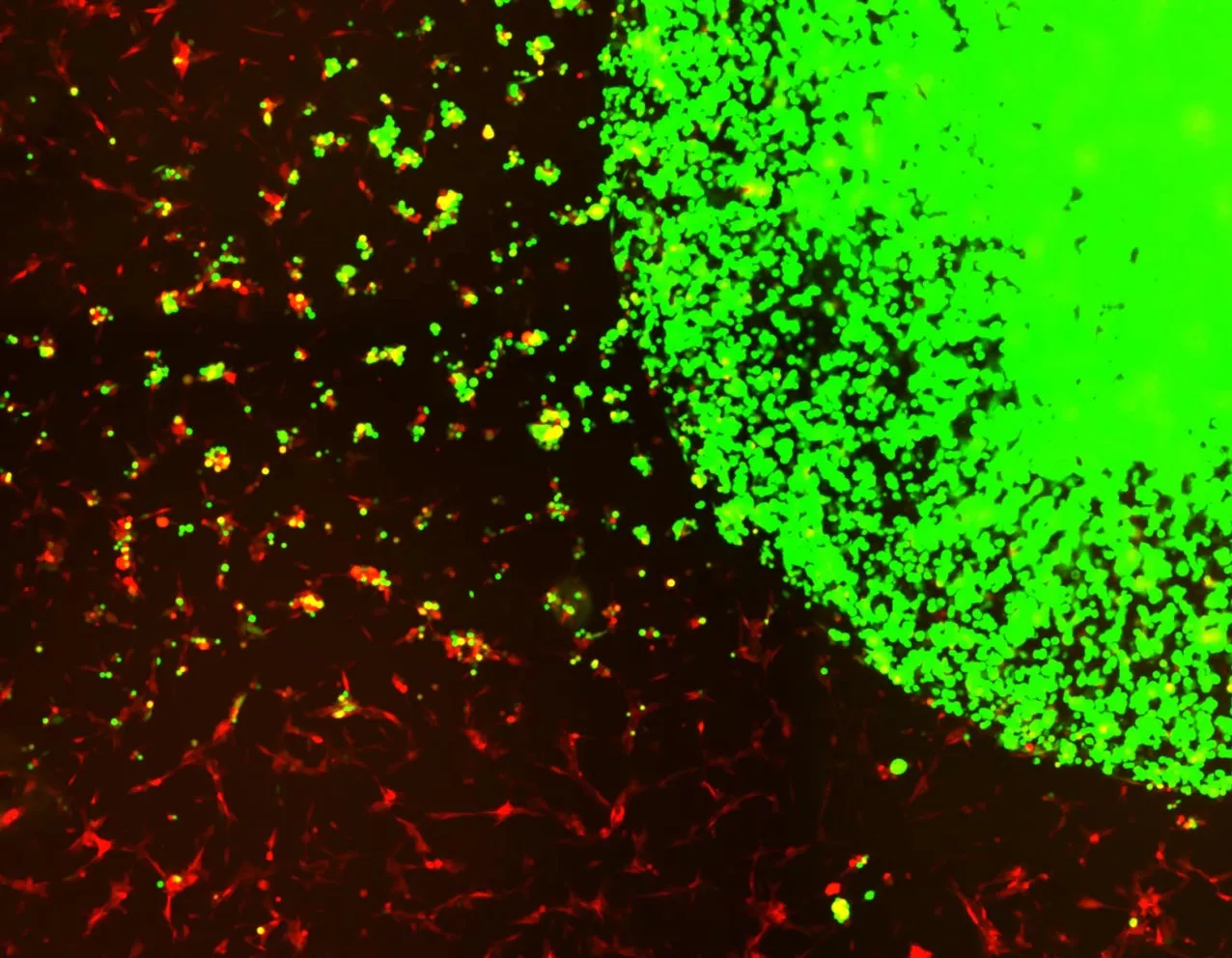
The researchers first identified specific receptors on circulating tumor cells (CTC) - or cancer cells in the blood. These receptors are called "death receptors", which use a genetic biomarker usually expressed on tumor cells. After identification, the researchers extracted stem cells from the bone marrow of healthy human donors and designed cells to release a protein that binds to the death receptor and initiate cell death. In addition, they have established a safety switch in the stem cell system that allows the tracking of stem cells through PET imaging. Once activated, it can eliminate stem cells and further enhance the death of cancer cells. Finally, Shah's team evaluated the efficacy of therapeutic bifunctional cells (mscbif) in animal models after surgery for primary and recurrent GBM tumors.
It should be noted that all mice treated with gel coated stem cells after surgery survived 90 days after treatment. Mice that underwent surgery alone showed an average survival time of 55 days. The researchers also evaluated the safety of this clinical treatment by treating mice with different doses of mesenchymal stem cells. They found no signs of toxicity in mice with or without tumors.
The findings of the study pave the way for phase I clinical trials in GBM patients undergoing brain surgery in the next two years. Shah and colleagues pointed out that this treatment strategy will be applicable to a wider range of solid tumors, and its application needs to be further investigated.
"In addition to the remarkable demonstrated success rate of this therapy, these findings suggest that we can use healthy human stem cells to treat cancer patients. This work lays a foundation for the establishment of an engineered therapeutic stem cell biobank for different receptors of tumor cells and immune cells in the tumor microenvironment, which will one day be used to treat a wide range of refractory cancers such as GBM," Shah said