It is estimated that type 1 diabetes affects about 1.8 million Americans. Although type 1 diabetes often occurs in children or adolescents, it may also occur in adulthood. Despite positive research, type 1 diabetes has not been cured. It is understood that the treatment includes taking islets, monitoring diet, managing blood glucose levels and regular exercise Scientists have also recently discovered a promising new treatment
A group of researchers from the University of Missouri, Georgia Institute of technology and Harvard University proved the successful application of a new type 1 diabetes treatment method in large animal models in a new study published in science advances on May 13. Their approach involves transferring insulin producing pancreatic cells, called islets, from donors to recipients without the need for long-term immunosuppressive drugs.
According to Haval shirwan, Professor of child health, molecular microbiology and immunology at the University of Maryland School of medicine and one of the main authors of the study, the immune system of patients with type 1 diabetes may malfunction and make them target themselves.
Shirwan said: "The immune system is a strictly controlled defense mechanism that ensures the well-being of individuals in an infected environment. When the immune system mistakenly identifies insulin producing cells in the pancreas as infections and destroys them, type 1 diabetes will occur. Usually, once the perceived danger or threat is eliminated, the command and control mechanism of the immune system will be activated to eliminate any rogue cells. However, if this machine If the system fails, diseases such as type 1 diabetes will appear. "
Diabetes impairs the body's ability to produce or use insulin, a hormone that helps regulate blood glucose metabolism. People with type 1 diabetes can't control their blood sugar levels because their bodies can't produce insulin. This lack of control can lead to life-threatening problems, including heart disease, kidney damage and loss of vision.
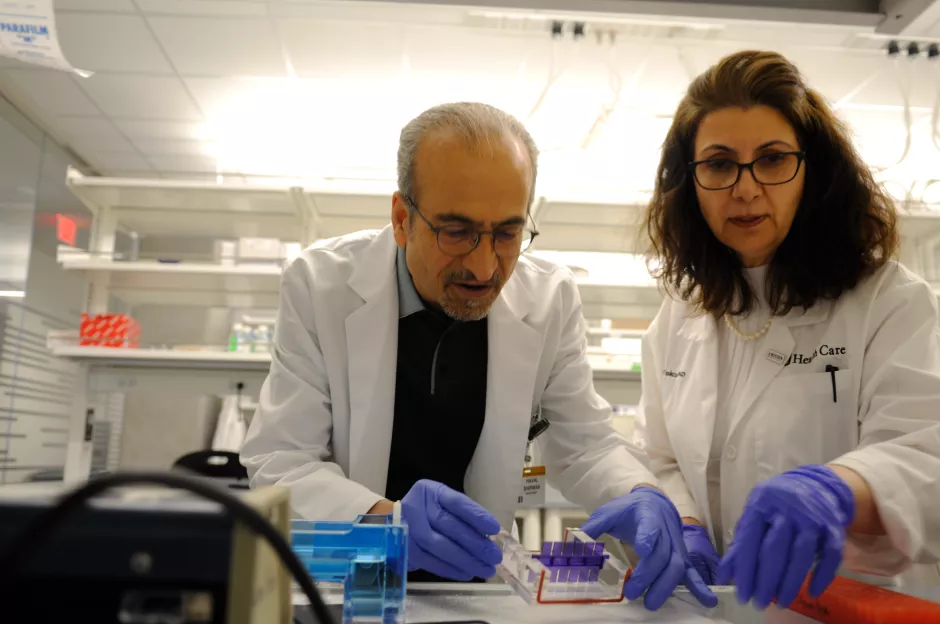
Shirwan and Esma yolcu, Professor of child health and molecular microbiology and immunology at Mu Medical College, have been studying a mechanism of apoptosis for the past 20 years. It is reported that this mechanism can prevent "rogue" immune cells from causing diabetes or rejecting transplanted islets by attaching a molecule called FasL to the surface of islets.
Yolcu, one of the first authors of the study, pointed out that: "When a molecule called FasL interacts with another molecule called Fas on rogue immune cells, a kind of cell apoptosis will occur and lead to their death. Therefore, our team created a technology that can produce a new type of FasL and present it on transplanted islet cells or micro gel to prevent rejection by rogue cells. After islet cells that produce insulin are transplanted, rogue cells are mobilized to the graft But it is eliminated by the Fas involved by the FasL on its surface. "
One advantage of this new method is that it is possible to give up the opportunity to take immunosuppressive drugs for a lifetime. These drugs, when introduced into the body, counteract the ability of the immune system to find and destroy foreign bodies, or in this case, avoid cell transplantation.
Shirwan said: "the main problem with immunosuppressive drugs is that they are not specific, so they may have many adverse effects, such as a high risk of cancer. Therefore, using our technology, we have found a way to regulate or train the immune system to accept, rather than reject these transplanted cells."
It is understood that their method uses the technology contained in the U.S. patents applied by the University of Louisville and Georgia Institute of technology. Since then, it has been authorized by a commercial company, which plans to seek FDA approval for human testing. In order to develop commercial products, researchers at the University of Maryland, in cooperation with Andres Garc í A and the Georgia Institute of technology, attached FasL to the surface of micro gel and proved its effectiveness in a small animal model. Then, they cooperated with Jim markmann and Ji Lei of Harvard University to evaluate the efficacy of FasL micro gel technology in a large animal model. The research report has been published.
Integrate the power of NextGen
This research is an important milestone in the research process of "from laboratory to bedside", that is, how the laboratory results can be directly used by patients to help treat different diseases, which is the symbol of MIT's most ambitious research program - NextGen precision health initiative.
NextGen precision health program emphasizes the commitment of personalized medical care and the impact of large-scale interdisciplinary cooperation. It brings together innovators from myitkya and the other three research universities of myitkya system, such as shirwan and yolcu, to pursue precision health progress that changes life. This is a cooperative effort to create a better future for the health of Missouri people and other regions by taking advantage of the research advantages of the University of Missouri. The Roy blunt NextGen precision health building of the University of Michigan is the foundation of the whole plan. In addition, it also expands the cooperation among researchers, clinicians and industry partners in the most advanced research facilities.
Yolcu said: "I believe that by using great facilities such as Roy blunt NextGen precision health building in the right institutions, we will be able to take the necessary steps based on the existing research results to further carry out the research and make the necessary improvements faster."
Shirwan and yolcu joined the Faculty of Michigan University in the spring of 2020. They are one of the first researchers to start working in NextGen precision health building. In addition, after nearly two years' work in Michigan University, they are now the first batch of NextGen researchers. Their research papers have been accepted and published in highly influential peer-reviewed academic journals.