A team of scientists from the University of Geneva has demonstrated how the "killer" T cells used to eliminate cancer cells in immunotherapy can also damage the lymphatic vessels of tumors, thus greatly reducing the risk of metastasis This synergistic effect can be used to improve the treatment of cancers that are important for lymphangiogenesis, such as colorectal cancer, melanoma or breast cancer. These results of researchers at the University of Geneva have been published in progress in science 》In magazines.
"Killer" T cells (also known as cytotoxic T cells or cytotoxic T lymphocytes) are immune cells that can kill certain cells, such as foreign cells, cancer cells and virus infected cells. Killer T cells can be isolated from other blood cells, cultured in the laboratory, and then injected into patients to kill cancer cells. Killer T cells are a type of white blood cells and a type of lymphocytes.
The lymphatic system is the main route for cancer cells to spread in vivo. They first colonize sentinel lymph nodes and then move to other parts of the body to produce secondary metastasis. So far, however, therapies that block tumor lymphangiogenesis have been disappointing. "In fact, they also represent a way for some immune cells (dendritic cells) to leave the tumor and activate anti-tumor killer T cells," explained St é Phanie Hugues, an associate professor of the Department of pathology and immunology of unige Medical College and the Geneva Center for inflammation research, who led the work. "Therefore, we must find a balance point to suppress this mechanism without completely blocking it, so as to interpret its mode of action in detail."
Identify a unique goal
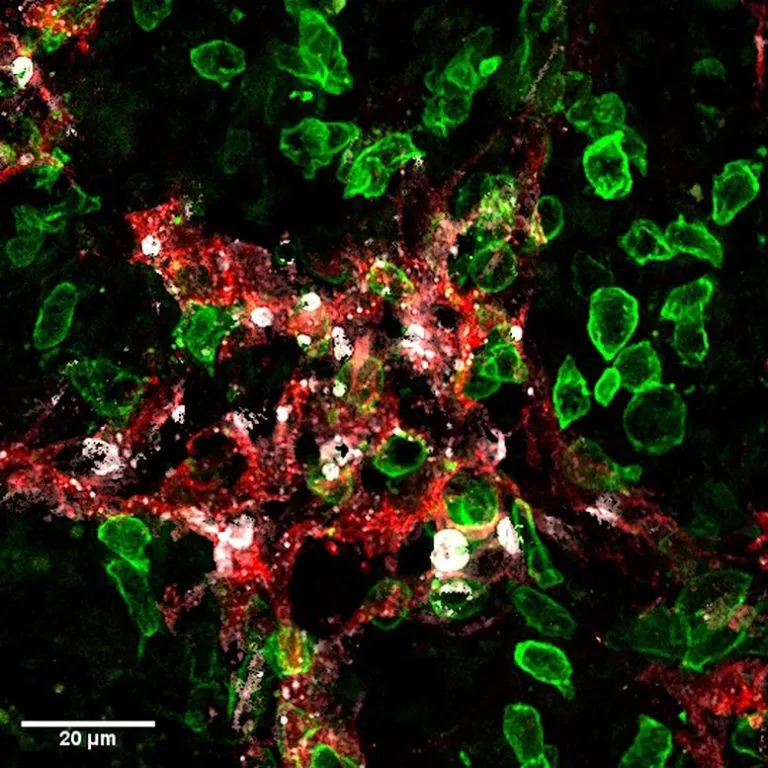
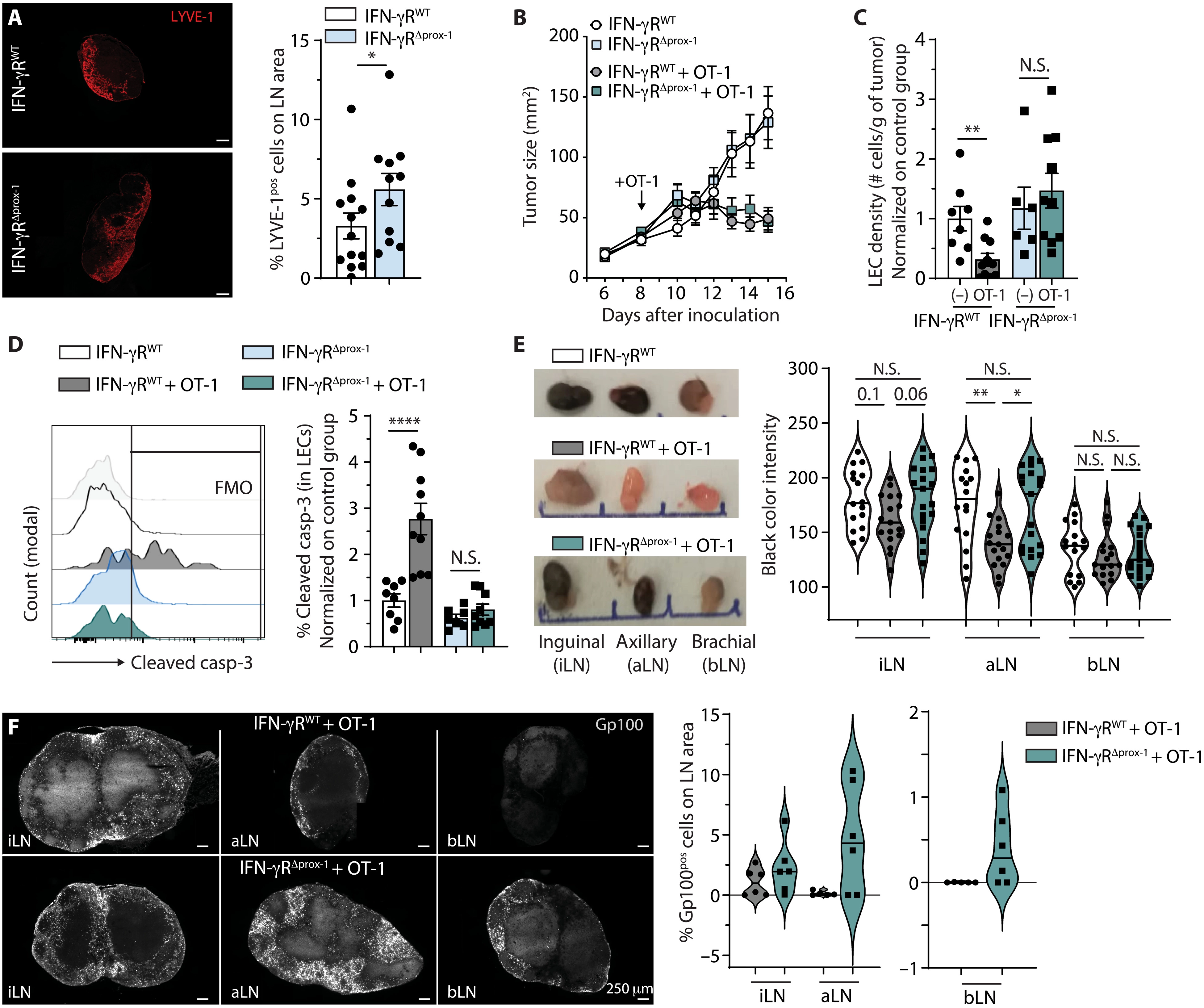
To do this, the scientists used the so-called "killer" T lymphocytes used in the immunotherapy regimen. Junior lecturer at St é Phanie Hugues laboratory Laure Garnier, the first author of this work, explained: "these T cells are immune cells specifically activated in the laboratory, used to eliminate tumor cells, and then injected into patients. Here, we inject them into mice with melanoma. If, as expected, killer lymphocytes destroy tumor cells, they also attack the lymphatic endothelial cells in the lymphatic vessels."
In fact, the destruction of cancer cells leads to the release of tumor antigens. These small cancerous parts are then captured by lymphatic endothelial cells, which, after becoming carriers of tumor recognition markers, are also recognized as enemies by the T cells attacking them. Thus, this mechanism disrupts the tumor associated lymphatic system, thereby greatly reducing the risk of metastasis without completely blocking it.
The team confirmed these results in other ways, such as vaccination aimed at strengthening the immune system. "We also observed the destruction of lymphatic endothelial cells, thus reducing lymph node metastasis, thus limiting the risk of secondary metastasis. In addition, since this effect only occurs in the tumor microenvironment, there is no need to worry about the systemic impact," Laure Garnier emphasized.
Increase synergy by selecting the right weapons
How to enhance this effect without impairing the action of immune cells, which need to enter the tumor through lymphatic vessels? There are several options, such as intervention after the establishment of immunity, or combination with treatment, because the immune system is very powerful and limiting lymphangiogenesis will not damage its function. St é Phanie Hugues said: "nevertheless, our results show that the most effective method is to use killer T cells generated in the laboratory, so it can be attacked at any time to bypass the first stage of activation, which may prove problematic."
Immunotherapy is still complex and should only be used if traditional therapies prove to be ineffective. "Even if they are very promising, these therapies are not miraculous solutions and often cause serious side effects. That is why we want to understand the smallest biological processes at work," the authors conclude.