More and more evidence shows that "long course covid", that is, several months after obvious recovery from severe covid-19, still has negative health effects, which is an important risk for some patients. For example, researchers at the University of Florida at Gainesville last December showed that hospitalized patients who seem to recover from severe covid-19 are more than twice as likely to die in the next year as those who have only mild or moderate symptoms, are not hospitalized or have never contracted the disease.
"It was found that the stronger the inflammation at the initial hospitalization, the greater the probability of death within 12 months after seemingly 'recovering' from covid-19."- Professor arch g mainous III
Now, for the first time, a research team, including some of the same authors, has shown that severe systemic inflammation during hospitalization is a risk factor for death within one year in patients hospitalized with covid-19 but who appear to have recovered. This seems contradictory, because inflammation is a natural part of the body's immune response, which evolved to fight infection. However, in some diseases, including covid-19, this response may go too far and cause further damage.
"Covid-19 is known to produce inflammation, especially in the first acute attack." "We are the first team to study the relationship between inflammation during covid-19 hospitalization and mortality after 'recovery'. Clinical observations show that the stronger the inflammation during the initial hospitalization, the greater the probability of patients dying within 12 months after seemingly 'recovery' from covid-19," said Professor arch g mainous III, the lead author and deputy director of research in the Department of community health and family medicine at the University of Florida Gainesville
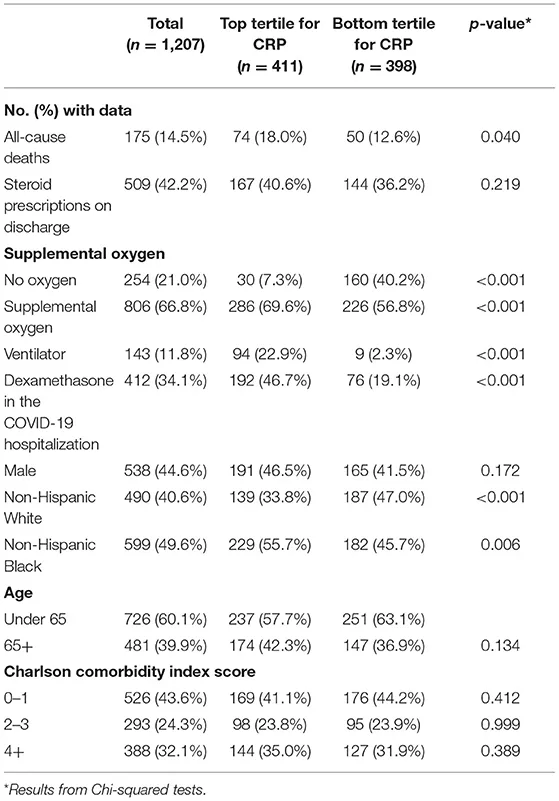
Mainous and colleagues studied the de identified electronic health records of 1207 adults hospitalized with covid-19 positive tests in the University of Florida health system in 2020 or 2021, who were tracked for at least a year after discharge. As a proxy for the severity of systemic inflammation during hospitalization, they used a common and proven measure, the concentration of C-reactive protein (CRP) molecules in the blood, which is secreted by the liver in response to signals from active immune cells.
Inflammation in many parts of the body
As expected, the blood concentration of CRP during hospitalization was closely related to the severity of covid-19. The CRP of inpatients who do not need supplemental oxygen is 59.4 mg / L, the CRP of patients who need additional oxygen through noninvasive and non-mechanical ventilation is 126.9 mg / L, and the most serious cases need ventilation through ventilator or through Yeke membrane oxygenation. The CRP demand is 201.2 mg / L.
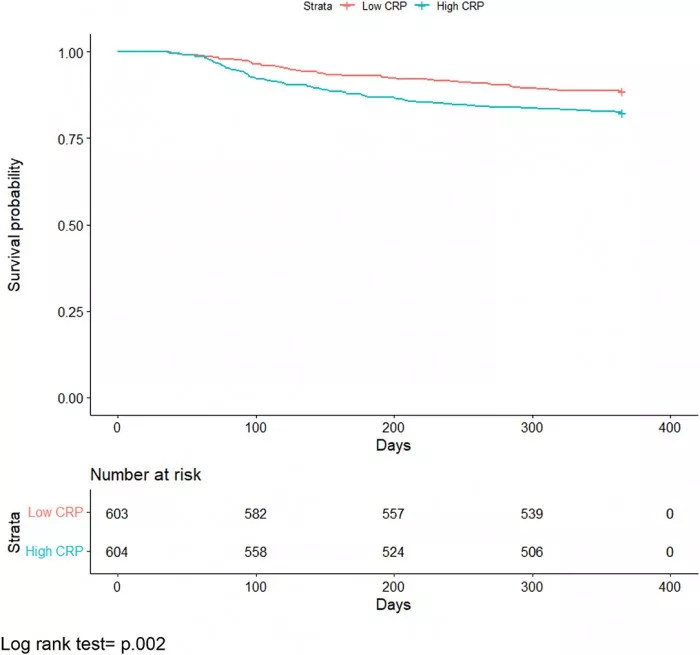
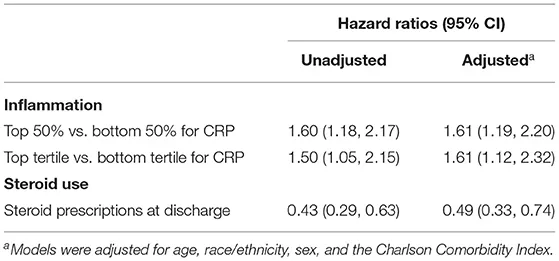
Covid-19 patients with the highest CRP concentration measured during hospitalization had a 61% greater risk of death from any cause within one year after discharge - adjusted for other risk factors - than patients with the lowest CRP concentration. These results were published in the journal frontiers in medicine on May 12, 2022.
Mainous said. "Many infectious diseases are accompanied by increased inflammation. Most of the time, inflammation is concentrated or specific to the infection. Covid-19 is different because it produces inflammation in many places except the respiratory tract, such as the heart, brain and kidney. High levels of inflammation can lead to tissue damage.". Importantly, the authors showed that if patients were prescribed anti-inflammatory steroids after hospitalization, the risk of death from causes associated with severe inflammation was reduced by 51%.
These results mean that the severity of inflammation during hospitalization for covid-19 can predict the risk of subsequent serious health problems, including the death of 'long course covid'. They also suggested that current best practice recommendations may need to be changed, including more widely prescribing oral steroids to covid-19 patients at discharge.
Covid-19: a chronic disease
The authors suggest that covid-19 should be considered as a potential chronic disease.
"When someone has a cold or even pneumonia, we usually think that once the patient recovers, the disease will end. This is different from a series of chronic diseases, such as congestive heart failure or diabetes, which continue to affect the patient after an acute attack." Mainous said: "we may also need to start thinking about the continued impact of covid-19 on many parts of the body after the patient recovers from the initial attack. Once we recognize the importance of 'long-term covid-19' after seemingly 'recovery', we need to focus on treatment to prevent subsequent problems, such as stroke, brain dysfunction, and especially premature death."