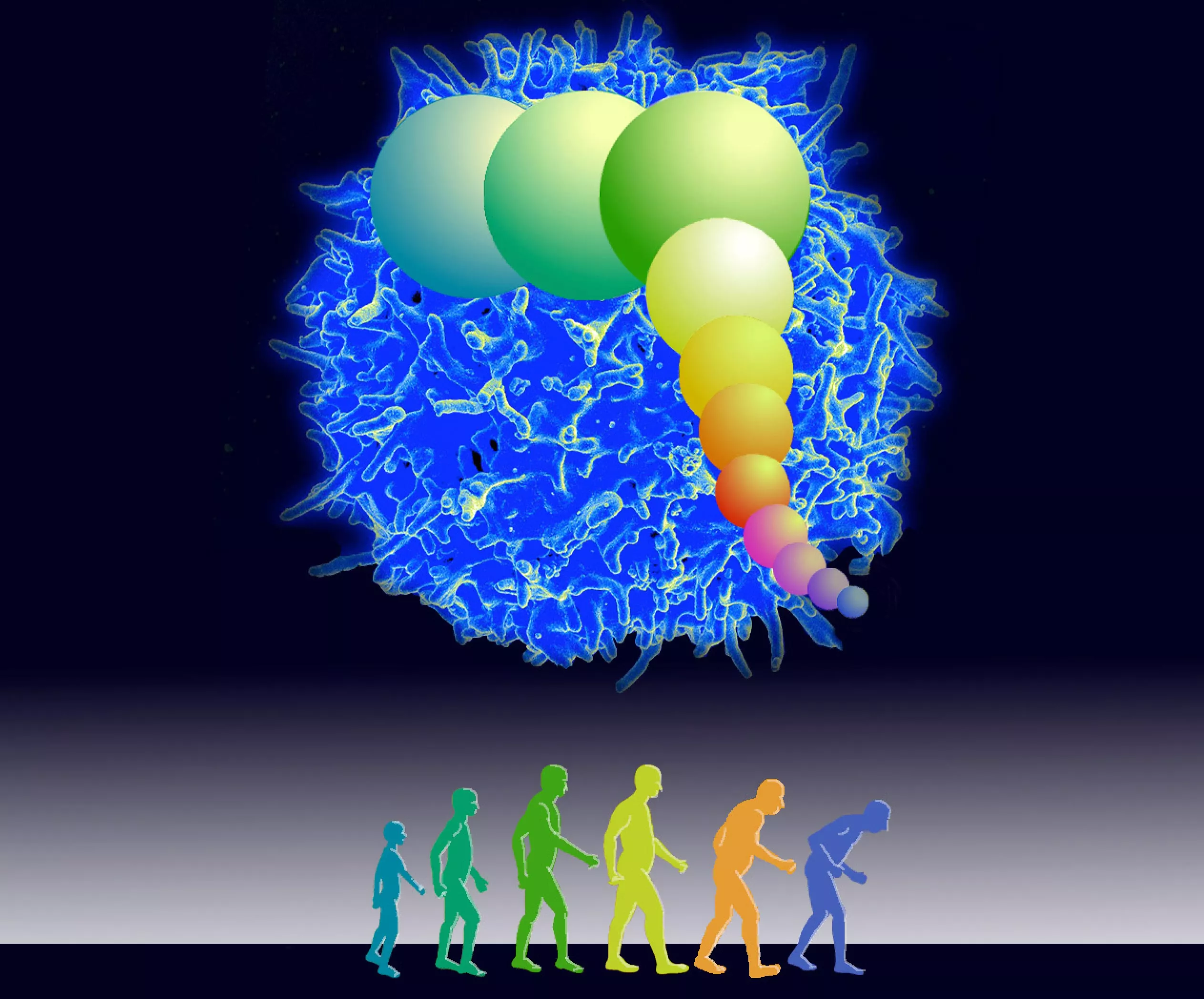
Like any infection, the ability of the human immune system to fight covid-19 mainly depends on its ability to replicate immune cells, which can effectively destroy the sars-cov-2 virus that causes the disease. However, these cloned immune cells cannot be created indefinitely, a new study from the University of Washington (UW) puts forward a key hypothesis that the body's ability to create these cloned cells will decline significantly in old age**
According to a new model created by UW Research Professor James Anderson, this genetic predetermined restriction on the human immune system may be the key to the devastating impact of covid-19 on the elderly. Anderson is the first author of a paper published in the lancet ebiomedicine on March 31, which details the model link between aging, covid-19 and mortality.
Anderson pointed out that when DNA divides during cell division, telomeres become shorter with each division. "After a series of replications, a cell becomes too short and stops dividing further. Not all cells or all animals have this restriction, but human immune cells have this cell life span". It is reported that Anderson is a biosystem modeler at the school of aquatic and Fishery Sciences.
Despite this limit, the average person's immune system is well maintained until about 50. Anderson said that at this time, enough core immune cells, namely T cells, have shortened telomeres, which can not quickly clone themselves through cell division, and then attack and eliminate covid-19 virus in a large enough number - which is characterized by a sharp reduction in the number of immune cells. In addition, Anderson added, it is important that telomere length is inherited from parents. Therefore, there are some differences in these lengths between people of each age group.
Anderson pointed out that the key difference between this understanding of aging - that is, there is a threshold for when the immune system runs out of collective telomere length - and the idea that everyone is aging over time is the most exciting finding in his study.
To build this model, the researchers used public data from the Centers for Disease Control and the U.S. Census Bureau on covid-19 mortality and telomere research.
Anderson said that gathering telomere length information about a person or a specific population can help doctors know who is less vulnerable. They can then allocate resources, such as booster needles, based on which groups and individuals may be more vulnerable to covid-19.
Anderson said: "I'm a modeler. I look at problems through mathematical equations. I work with biologists to explain them, but biologists need to look at information through models to guide their research problems. A modeler's dream is to really influence great biologists and make them think like modelers. But it's difficult."
In addition, Anderson also issued a warning to the model: "a large amount of data supports every parameter of the model, and there is a good logical idea about how you can model from the data channel. But it is so simple and intuitive that we should also be skeptical about it. As a scientist, I hope we can start to learn more about the immune system and group response as part of natural selection."