According to a new study by the University of Birmingham and the National Institutes of health, the use of immune promoting drugs in combination with antibiotics can reduce the health risk of complex infections Life threatening fungal infections invasive candidiasis is a major complication of hospitalized patients who are given antibiotics to prevent sepsis and other bacterial infections that spread rapidly in the hospital (e.g. C. diff). Fungal infections may be more difficult to treat than bacterial infections, but the basic factors leading to these infections are unclear.
Candidiasis is a fungal infection caused by a yeast called Candida (a kind of fungus). Some kinds of Candida can cause human infection; The most common is Candida albicans. Candida usually appears on the skin and some parts of the body, such as the mouth, throat, intestines and vagina, and will not cause any problems. If Candida grows out of control or goes deep into the body (for example, blood or internal organs, such as kidneys, heart or brain), it can cause infection.
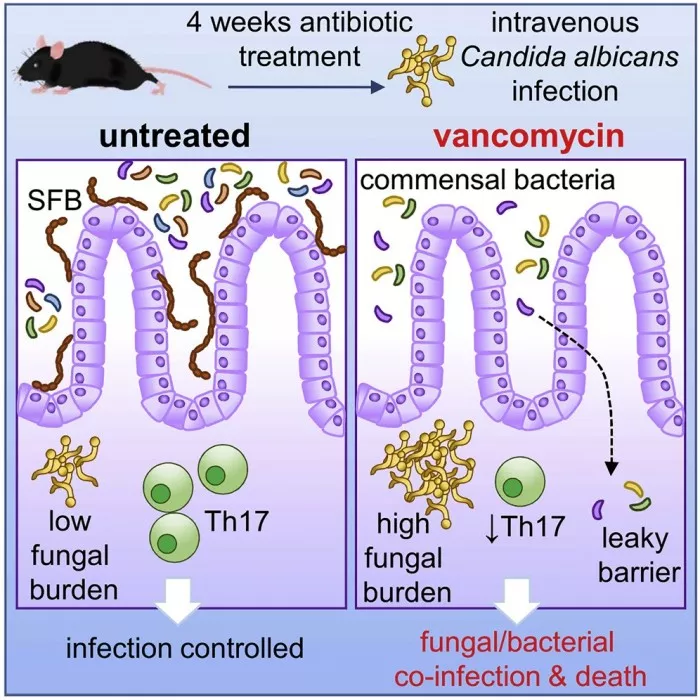
A team from the University's Institute of immunology and immunotherapy, together with researchers from the National Institutes of health, found that antibiotics disturbed the intestinal immune system, which means that the control of fungal infection in the region is not effective. Unexpectedly, the team also found that intestinal bacteria could escape where fungal infections occurred, resulting in an additional risk of bacterial infection.
Published in cell, host and microorganism 》The study on shows the potential of immune promoting drugs, but the researchers also say their work also highlights how antibiotics have additional effects on our bodies and how we fight infections and diseases. This in turn emphasizes the importance of careful management of existing antibiotics.
Lead author Dr Rebecca Drummond said: "we know that antibiotics can worsen fungal infections, but it is surprising to find that bacterial co infections can also develop through these interactions in the intestine. These factors together can form a complex clinical situation - by understanding these root causes, doctors will be able to treat these patients better and effectively."
In this study, the team used mice treated with a "cocktail" of broad-spectrum antibiotics and then infected the animals with Candida albicans, the most common fungus that causes invasive candidiasis in humans. They found that although the mortality of infected mice increased, it was caused by intestinal infection, not kidneys or other organs.
In further research, the team determined which parts of the immune system were missing from the intestine after antibiotic treatment, and then reintroduced them into mice using immune promoting drugs similar to those used in humans. They found that this method helped reduce the severity of fungal infections.
The researchers followed the experiment by studying hospital records. Their research can show that humans may have similar co infections after receiving antibiotics.
Dr Drummond added: "these findings suggest that the use of antibiotics in patients at risk of fungal infection may have consequences. If we limit or change the way we prescribe antibiotics, we can help reduce the number of people who are terminally ill due to these additional infections - and address the huge and growing problem of antibiotic resistance."