A new study from Dr. Ben Philpot's Laboratory of UNC Neuroscience Center found that in the animal model of Peter Hopkins syndrome (a rare single gene neurodevelopmental disease), the restoration of lost gene activity can prevent many disease symptoms. Peter Hopkins syndrome is a rare genetic disease caused by mutations in the Tcf4 gene on chromosome 18.
Peter Hopkins syndrome is characterized by stunting, underlying respiratory problems such as paroxysmal hyperventilation and / or holding your breath while awake, recurrent seizures / epilepsy, gastrointestinal dysfunction, lack of language ability, and unique facial features. Children diagnosed with Peter Hopkins syndrome often have a happy and lively attitude, often smiling and laughing.
The incidence rate of Peter Hopkins syndrome in the general population is unknown. However, some estimates suggest that the incidence rate of Peter Hopkins syndrome ranges from 1 in 34000 to 1 in 41000. The disease affects both men and women and is not limited to a single ethnic group.
Peter Hopkins syndrome is classified as an autism spectrum disorder, and some patients are diagnosed with autism, "atypical" autism features, and / or sensory integration dysfunction. Many researchers believe that due to the genetic link between Peter Hopkins syndrome and autism and other diseases, the treatment of Peter Hopkins syndrome will lead to the treatment of similar diseases.
Researchers from the University of North Carolina School of medicine have shown for the first time that postpartum gene therapy may be able to prevent or reverse many negative effects of Peter Hopkins syndrome, a rare genetic disease. Severe growth retardation, mental retardation, respiratory and motor abnormalities, anxiety, epilepsy, and moderate but significant facial abnormalities are all symptoms of this autism spectrum disorder.
Scientists published their findings in the Journal eLife. They created an experimental gene therapy like technology to restore the normal function of gene defects in patients with Peter Hopkins syndrome. This drug treatment prevented the occurrence of disease indicators, such as anxiety like behavior, memory impairment, and abnormal gene expression patterns in affected brain cells in newborn mice, which would otherwise become a model of the syndrome.
Dr. Ben Philpot, senior author, Kenan distinguished professor of cell biology and physiology at UNC School of medicine and deputy director of UNC Neuroscience Center, said: "this first principled proof shows that restoring the normal level of Peter Hopkins syndrome related genes is a feasible treatment, otherwise there is no specific treatment."
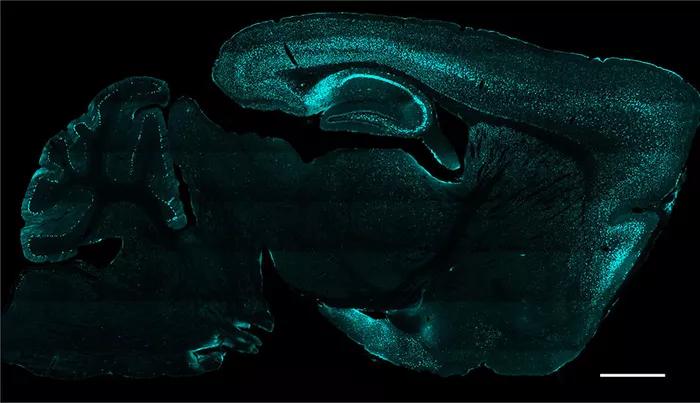
Brain slice image: protein CRE (green) is delivered to cells through AAV as gene therapy. Source: philport Laboratory (UNC School of Medicine).
Most genes are inherited in pairs, one from the mother and one from the father. When a copy of Tcf4 gene is missing or mutated, resulting in insufficient Tcf4 protein level, Peter Hopkins syndrome will appear in children. Usually, this deletion or mutation occurs spontaneously in the eggs or sperm cells of the parents before conception, or in the early stages of embryonic life after conception.
Since Australian researchers first described the syndrome in 1978, only about 500 cases of the syndrome have been reported worldwide. But no one knows the true prevalence of the syndrome; Some estimates suggest that there may be more than 10000 cases in the United States alone.
As Tcf4 is a "transcription factor" gene, it is the master switch that controls the activities of at least hundreds of other genes. It is destroyed from the beginning of development, resulting in many developmental abnormalities. In principle, preventing these abnormalities by restoring normal Tcf4 expression as soon as possible is the best treatment strategy -- but it has not been tested.
Under the leadership of the first author Dr. hyojin (Sally) Kim (a graduate student in Philpot laboratory during the study), Philpot's team developed a mouse model of Peter Hopkins syndrome, in which the level of Tcf4 in the mouse version can be reliably halved. This mouse model shows many typical symptoms of the disease. Restoring the full activity of this gene from the embryonic stage can completely prevent these symptoms. The researchers also found in these initial experiments that basically all types of neurons need to restore genetic activity to prevent the emergence of Peter Hopkins disease.
Next, the researchers established a proof of concept experiment to simulate real-world gene therapy strategies. In engineering mice, about half of the mouse version of Tcf4 expression was turned off. Researchers used a virus transmitted enzyme to turn on the missing expression again in neurons when the mice were born. Analysis of the brain showed that this activity was restored in the next few weeks.
Although the brain and body of the treated mice were moderately smaller than those of normal mice, they did not show many abnormal behaviors in untreated Peter Hopkins model mice. The exception was the innate nesting behavior, and the treated mice seemed abnormal at first, although their ability returned to normal within a few weeks.
The treatment at least partially reversed two other abnormalities seen in untreated mice: changes in gene levels regulated by Tcf4 and changes in neuronal activity patterns measured in electroencephalogram (EEG) recordings.
"These findings provide hope that future gene therapy will provide significant benefits to people with Peter Hopkins syndrome, even after birth; it will not require in utero diagnosis and treatment," Kim said
Philpot and his lab now plan to explore the effectiveness of their strategy when applied to Peter Hopkins mice at a later stage of life. They also plan to develop an experimental gene therapy, in which the human Tcf4 gene itself will be transmitted to the Pitt Hopkins mouse model through the virus - a treatment that can eventually be tested in children with Pitt Hopkins syndrome.
"The results here suggest that there are other ways to restore Tcf4 that can work, including treatments that increase the activity of the remaining, good copies of Tcf4," Philpot said
This study was supported by ANN D. Bornstein of the Peter Hopkins research foundation, the National Institute of neurological diseases and stroke (r01ns114086), the Estonian Research Council, and the orphan disease center of the Perelman School of medicine at the University of Pennsylvania (mdbr-21-105- Peter Hopkins).