According to a new analysis by scientists from Yale University and wasa college, although the U.S. spends twice as much on cancer care as the average high-income country, its cancer mortality rate is only slightly better than the average The results were published in [American Medical Association Health Forum] on May 27, 2022( https://jamanetwork.com/journals/jama-health-forum/fullarticle/2792761 ) 》In magazines.
"It is generally believed that the United States provides the world's most advanced cancer care," said Ryan Chow, M.D., Yale University, the lead author. "Our system is touted as developing new treatments and providing them to patients faster than other countries. We are curious whether the large investment in cancer care in the United States is really related to better cancer outcomes."
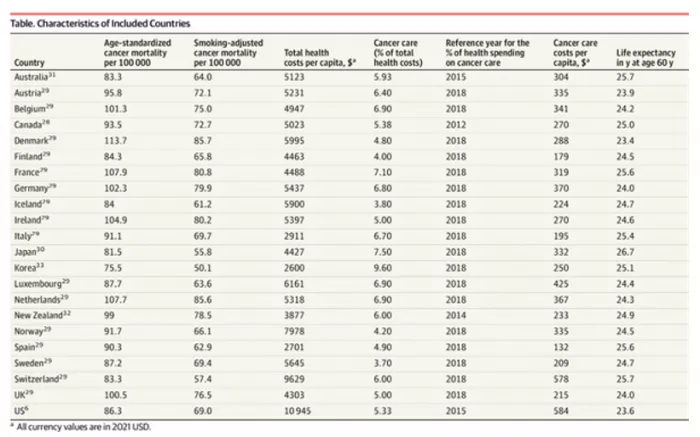
Of the 22 high-income countries included in the study, the United States had the highest expenditure rate.
Cary gross, senior author, Professor of medicine at Yale University and director of the national clinicians program, said: "the United States spends more than $200billion a year on cancer care - about $600 per person, compared with $300 per person in other high-income countries. This raises a key question. Is our money worth it?"
The researchers found that there was no relationship between national cancer care expenditure and cancer mortality at the population level. "In other words, countries that spend more on cancer care do not necessarily have better cancer outcomes," Chow said
In fact, six countries - Australia, Finland, Iceland, Japan, South Korea, and Switzerland - have lower cancer mortality and costs than the United States.
Smoking is the strongest risk factor for cancer death. Compared with other countries, the smoking rate in the United States has always been relatively low. When researchers controlled for international differences in smoking rates, cancer mortality in the United States became no different from that in general high-income countries. Nine countries - Australia, Finland, Iceland, Japan, South Korea, Luxembourg, Norway, Spain and Switzerland - had lower smoking adjusted cancer mortality than the United States.
Chow said: "after adjusting for smoking, the situation in the United States is more unfavorable because the low smoking rate in the United States has a protective effect on cancer mortality."
The authors say that more research is needed to identify specific policy interventions to meaningfully reform the U.S. cancer care system. However, they pointed out that lax regulation of cancer drug approval and drug pricing are two key factors leading to the high cost of cancer care in the United States.
Elizabeth Bradley, co-author, Dean of wasa college and professor of science, technology and society, said: "in the U.S. health care system, the model of spending more and getting less is well documented; now we see this in cancer care. If we are willing to change, other countries and systems have a lot to teach the United States."